|
Site outline: |
|
This level:
|
|
Subpages: |
|
|
|
"Some things are meant to be given
away for free. The IPT method is one of them."
The current method, in detail. A PowerPoint slide show demonstrating the current method An IPT Training Program is now available for medical doctors through Donato Perez Garcia, M.D. 3.
Here, in detail, are the steps of the current IPT procedure:
2. Doctor Preparation. The doctor may request that the patient have more tests done or images taken. Then, based on all the information at hand, the doctor puts together a treatment plan, and decides on the medications to be given during the first treatment. 3. Choice of medications. Intravenous insulin and hypertonic glucose are the common elements of all IPT treatments. Insulin type and dose may be varied to determine the speed and depth of hypoglycemia. A larger dose goes faster and deeper. The insulin of choice is currently Humalog ® (Lilly) fast-acting lispro insulin, given at 0.1 to 0.4 units per kilogram of patient weight. (This is the range of doses specified in the 1990 patent. Preferred doses, which tend towards the upper end of this range, are explained by Dr. Perez Garcia 3 during training.) Formerly, Humulin ® (Lilly) human-like insulin was used, in the same dosage. Typically 20 cc of 50% hypertonic glucose is given later in the treatment (see below). But the real art is in the choice and dosage of the other medications. Typically they consist of:
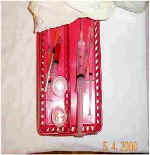
Medications packaged for any delivery method can be used. Typically they include oral, intravenous, and intramuscular compositions. A typical treatment may incorporate from 5 to 25 different medications. It should be noted that the Drs. Perez Garcia and Dr. Paquette have empirically found certain medications and combinations to be particularly useful in combination with IPT. Many of these are disclosed in the 1990 and 1992 patents, and in Medicine of Hope. Others are disclosed during training by Dr. Perez Garcia 3, and by consultation with him and the other experienced IPT doctors. 4. Patient Preparation. The patient is encouraged to take 25ml of lactulose syrup (a laxative) after breakfast on the day before the treatment, to help detoxify the digestive system. The patient can have lunch and dinner as usual, and then begins fasting after dinner that night. No food after 11 pm. Sometimes the patient is also directed to take a laxative that evening, to clear the bowels before the treatment in the morning. On the morning of the treatment, only water is permitted --- no breakfast and no medications. Dr. Perez Garcia 3 is particularly sensitive to patient comfort. He avoids extra tests and blood draws whenever possible. In an email he wrote me: "I just don't like to torture more these suffering humans. That is why I always make a joke about the procedure or something that would relieve the patient's tension. Even a hug helps a lot." The patient comes to the office in the morning, gets into a hospital gown (for comfort and to avoid absorbing sweat into the clothing), and is placed into a comfortable bed. A standard intravenous (IV) saline drip (250 cc of NaCl 0.09%) is installed in an arm vein. This makes the injection of insulin, glucose, and other intravenous medications very easy. And it adds to the safety of the procedure by allowing for very quick administration of glucose if the patient over reacts to insulin, without having to search for a vein. 5. Preparation of Medications. Typically done shortly before the treatment, either by the doctor, or by a highly trained nurse according to the doctor's prescription. Medications are opened, mixed, dosed, and laid out systematically on a tray. Intramuscular drug syringes with proper doses are placed together. Oral medications are placed together. And intravenous medications in syringes are placed together. This way all the medications can be administered quickly and systematically. It is a good idea to have extra glucose ready, in case the procedure needs to be terminated quickly. Water is needed for taking oral medications. And a sugar-sweetened drink (preferably Gatorade ®) is needed for recovery. 6. Insulin Injection, and IM and oral medications. Insulin is injected into the IV line. These days, this is usually Humalog ® (Lilly) fast acting insulin, typically 0.1 to 0.4 units per kilogram of patient weight. A larger dose leads to faster and deeper hypoglycemia, and 0.4 units/kg is the most common dose today. Formerly, Humulin ® (Lilly) was the preferred insulin, given in a similar dose, and requiring a longer time to develop hypoglycemia. It is important to immediately write the time of insulin administration on the IV bag, to avoid any possible confusion. A few minutes after insulin administration, the oral medications are taken with water, and the intramuscular (IM) drugs are injected into the buttocks. These medications are given approximately 5 to 18 minutes after Humalog administration, or some 10 to 20 minutes after Humulin administration. Exact timing is based on clinical observation of the patient, and the doctor's judgment based on experience. Oral and IM medications are taken at this early stage because they take longer to absorb into the bloodstream (IV medications are absorbed instantly later in the treatment). 7. Waiting and observation. Under close observation by the doctor, or a highly trained nurse, the patient just relaxes and waits for the insulin to take effect. Gradually, symptoms of mild hypoglycemia develop, at a speed that depends on type and dose of insulin, and individual patient response, This can take about 18 to 21 minutes for Humalog , and about 20 to 40 minutes for Humulin, depending on dose, patient symptoms, and the doctor's judgment. These symptoms can include increased body temperature, palpitation and tachycardia (slightly irregular or faster heartbeat), hunger, thirst, mild sweating, and often sleepiness. Normal blood sugar ranges from about 80 to 100 mg%. The target range for mild hypoglycemia in IPT is about 25 to 45 mg/dL, as measured on a glucometer, high enough that the brain is not deprived of glucose. In Mexico, doctors often do not need to take blood samples for monitoring blood sugar levels, but only needs to carefully watch for the symptoms. This skill becomes better with years of practice. In the US, and as taught at IPT seminars, blood glucose measurements are taken at the time of insulin administration, at the apparent therapeutic moment, and after the glucose and sweet drink at the end. If symptoms were ever to develop too fast or go too far, due to unexpected hypersensitivity of the patient to insulin, or due to other causes, 20 cc of 50% hypertonic glucose (more if needed) could be immediately injected IV to quickly bring symptoms to a halt, and end the treatment. Glucose is always kept ready for such an unlikely situation, the same way fire extinguishers are kept ready for an unlikely fire. (Situations like this are very rare. Dr. Perez Garcia 3 has only experienced this once, and that was due to the nurse not properly noting the time of insulin injection. There was no harm to the patient, just anxiety of the medical team as they tried to find out what had happened.) 8. "The Therapeutic Moment." This is the point where the body has become prepared to receive all the medications into its cells and tissues. The hypoglycemia has reached the level the doctor wishes, as determined by his monitoring of the patient's symptoms. And the oral and intramuscular medications have been absorbed enough into the bloodstream. "The doors to the cells are open," as the Drs. Perez Garcia have long expressed it. Symptomatically, Dr. Perez Garcia 3 recognizes this moment by "when the patient says 'I am hot'." At this point the intravenous medications are administered into the IV line. They are followed immediately by the 20 cc of 50% glucose, either directly into the line (faster), or mixed into the IV bag (slower). This quick choreography apparently delivers all the medications simultaneously into all tissues and cells of the body, even into parts that are normally difficult to penetrate. 9. Recovery. The hypoglycemia immediately recedes, and symptoms end, as the glucose is quickly distributed through the body. This takes only a few seconds, regardless of the type of insulin used. (This is quite an amazing transformation to experience the for first time, whether you are the patient or the doctor.) The patient is then given a sugar-sweetened drink (preferably 16 oz of Gatorade ®) as desired to complete bringing the blood sugar back to normal. After 60 to 90 minutes, the patient can get dressed, and then goes to the doctor for follow-up instructions. The entire procedure may have taken as little as 90 minutes, if Humalog ® insulin was used. 10. Follow-up. After the treatment, the doctor asks the patient about how they feel, and about any improvement of symptoms. The patient is instructed to follow a healthy low-fat high-fiber diet, drink juices, take a mild fiber laxative (cancer patients take lactulose), practice good sleeping habits, avoid smoking and smokers, and get mild regular exercise. And the only alcohol allowed is 2 to 4 ounces of red wine 3 to 4 times per week. Then the patient is sent off to have a fresh fruit salad (which he will be hungry for). Lunch and dinner can be eaten later that day, but no spicy or fatty foods. The patient does not return to the office until the next IPT treatment. 11. Medications between treatments. In many cases, the doctor will prescribe oral medications for the patient to take between treatments. The dose is typically less than normal, but not as low as would be given during an IPT treatment. 12. Timing of treatments. Timing of treatments is highly variable, depending on the disease and condition of the patient, how the patient is responding, patient convenience (travel and lodging arrangements), and the doctor's experience with similar cases. Typically IPT treatments for cancer can be given one to five times the first week or two, then weekly for a few months, then monthly until complete remission is obtained. Arthritis may require just one to three treatments, often with complete remission for about 5 to 7 years, at which time treatments can be repeated. 13. Progress of tumors. According to Dr. Perez Garcia, tumors often stop growing after the first few treatments, but may not start shrinking until after 8 or 10 treatments, and may need as many as 24 treatments to become "almost completely invisible". When laboratory studies of IPT are finally carried out, we will find out what is going on inside tumors during this process.
|